What does high quality, trustworthy V1C look like? Explore the IMPACT Core Competencies framework to discover what good V1C looks like and how to get there.
Core Competency: Clinical & Operational Integration
Fits seamlessly within an individual’s larger healthcare context
- Seamless patient onboarding process
- Ability to navigate patients to downstream services
- Positioned for clinical integration with other sites of care and providers
- Positioned for operational integration with other platforms and healthcare benefits
Exceptional V1C entities are characterized by their ability to connect the dots – operationally and clinically – for patients and partners across a patient journey and between providers and care settings. They consider patient care as a holistic journey rather than a transaction and invest intentionally in data analytics and interoperability, clinical workflows and wrap-around services, and collaborations that position them to facilitate seamless transitions of care into, between, and out of V1C care.
- Patients
- Payers
- Health Systems & Providers
- Employers
- Investors
Value providers who take their past medical history and entire health status into account and trust that providers are talking to one another.
Health plans value V1C solutions that cover the breadth of services required to treat the ‘whole person.’ Operational and clinical integration means improved member experience across the care journey and, where needed, coordination between providers that reduces duplication of services, and reduces delays and costs due to avoidable specialist referrals and exacerbations leading to urgent care or preventable hospitalizations. Payers still want patients to have a medical home and seek complementary V1C services that don’t abrade existing providers in their network.
Traditional and emerging health systems (e.g., ACOs) seek V1C partnerships that are complementary: effectively filling in gaps in care and augmenting their services without competing, whether this is faster access to specialists or 24/7 urgent care. Clinical integration powered by data interoperability, two-way sharing, and formal and informal partnerships enables health systems to retain patients while maintaining or improving safety, quality, timeliness of care, and satisfaction for both their providers and patients.
Employers are increasingly charged with keeping up with their workforce’s changing needs and demands. On the one hand, employees are managing significant burdens of chronic disease, and on the other wanting to be taken care of more holistically than past generations. Although employers are leaning toward virtual care solutions, they are frustrated by low utilization, duplication of services, and patient confusion over benefits. They value providers who deliver best-in-class customer services, are adept at attracting and retaining eligible members, and are positioned to help navigate patients to covered benefits and services outside of their own practice.
Funders expect stage V1C providers to demonstrate how they logically fit into the larger health system. These ventures have a higher potential to scale beyond niche markets into the employer, health system, and insurance networks.
Maturity: Emerging
To realize the full potential of V1C this new care delivery model must be integrated, clinically and operationally into the existing healthcare system adding value to patients, providers, and payors by improving the experience and health outcomes and economic sustainability of healthcare overall. As the ‘newcomer’ on the scene, V1C providers risk adding to the already chaotic and fragmented patient experience if they can’t meet the market where it is at. Thus, V1Cs must demonstrate that they can work well within a system of care that spans an entire patient journey.
As patients’ conditions and care needs change throughout the course of their illness, their care may transition between different settings, sites of care, and practitioners. High quality V1C providers invest intentionally in workflows, data systems, and partnerships that minimize friction as patients transition into, between, and out of V1C.
Characteristics of seamless care transitions:
- Occur in clinically relevant timeframes
- Enable exchange of appropriate information between the right parties
- Make efficient use of health resources, including services and clinical workforce, avoiding duplication of services
- Minimize inconvenience and disruption to patients
- Produce optimal patient outcomes
Important V1C Care Transitions Along the Patient Journey
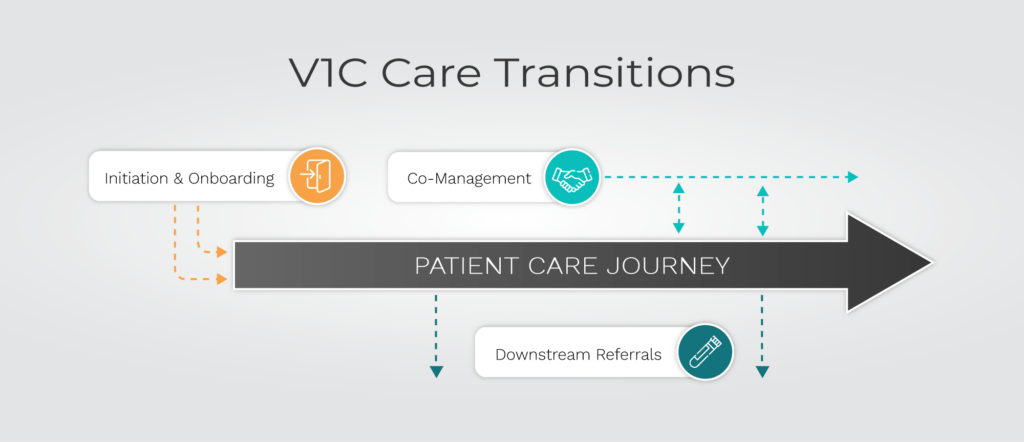
Click to learn more about the stages of V1C Care Transitions.
Patients and care partners have the education and technology support to access and use virtual care platforms.
Intake processes are supported by intentional workflows and a tech stack that facilitate:
- Insurance eligibility and coverage, including plan-specific copays and incentives
- Integration and digestion of current and past clinical records, including demographics, diagnoses, comorbidities, and procedures
- Medication reconciliation, including updating information and verifying with patients
- Mapping informal care partner roster
- Integrating relevant patient-generated data from digital technologies and surveys
Emerging Gold Standard Practices
- The use of advanced data science (AI, ML, or NLP, as applicable) and digital assessments enables the practice to personalize a patient experience and streamline triage to the appropriate setting and provider for their needs, and escalate care when required.
Resources
- Guide to Effective Virtual-First Care (V1C) Care Transitions
- A Tech Stack for Effective V1C Care Transitions
- Engaging Informal Care Partners for Optimal V1C Care Transitions
- Conceptualizing a Data Infrastructure for the Capture, Use, and Sharing of Patient-Generated Health Data in Care Delivery and Research through 2024
Case Studies
- Biofourmis Case Study: Coordinating Virtual Specialty Care for Polychronic Patients
- Byteflies Case Study: Digital Medicine as an Enabler of Effective V1C Care Transitions
- Freespira Case Study: Virtual Care Partnership Provides Mental Health Care for Managed Medicaid Members
- Heartbeat Health Case Study: V1C Partnering with ACOs for Effective Care Transitions
- Oshi Health Case Study: Achieving Whole-Person Care
- Thirty Madison Case Study: Seamless Downstream Referrals Advance Access to HIV Prevention
- Wellinks Case Study: Integrating High-Value V1C Solutions for Disease Management
High patient participation in referred services and completed orders (e.g, scheduled and resulted diagnostic tests and fulfilled prescriptions)
Patients are highly satisfied with downstream services
Timely and convenient scheduling, delivery of tests or medications, test results, and interpretations
Avoidance of excessive patient out-of-pocket costs or absorbed costs for practice
Emerging Gold Standard Practices
Partnerships, technologies, and decision algorithms are in place to ensure that clinicians and care teams can navigate available options and have a scalable process for guiding patients to services with considerations for:
- Availability of appropriate downstream care services: Uses modern technology platforms and payor relationships to identify clinically relevant services available locally in a clinically relevant timeframe. It specifically solves the problem of how to get services to patients with limited mobility and those in rural communities
- Payment and business model impact: Models end-to-end pathways and patient scenarios to understand the factors affecting patient and practice costs of various choices
- Value: Invest in tools and partnerships to identify the highest quality and best prices; this might involve collaborating with health plans to leverage their high-value networks
- Patient preference: Ensure fulfillment of care plans by considering individual patient preferences and access, including the ability to afford copays
- Provider workflow: Select interoperability technology and vendor relationships that ease ordering and scheduling burden
Resources
- Guide to Effective Virtual-First Care (V1C) Care Transitions
- A Tech Stack for Effective V1C Care Transitions
Case Studies
- Biofourmis Case Study: Coordinating Virtual Specialty Care for Polychronic Patients
- CareHive Case Study: Navigating Patients across the Continuum of Care Transitions
- Heartbeat Health Case Study: Leveraging In-Home Care Providers to Address the “Last Mile of Care”
- Heartbeat Health Case Study: V1C Partnering with ACOs for Effective Care Transitions
- Oshi Health Case Study: Achieving Whole-Person Care
- Thirty Madison Case Study: Seamless Downstream Referrals Advance Access to HIV Prevention
Positioned for bi-directional communication & information flow with clinical partners:
- Uses Fast Healthcare Interoperability Resources (FHIR) standards for seamless Application Programming Interface (API) integration, evidence-based clinical protocols
No evidence of redundant diagnostic testing or procedures
Minimal delays in decision-making and treatment due to insufficient/inaccessible data and information
Emerging Gold Standards
Positioned to collaborate with other V1C and bricks-and-mortar providers to advance shared quality and efficiency goals at the patient and population level:
- Patients, care partners, and co-managing clinicians can access current care plans easily
- Uses standard workflows to reconcile potential care and medication conflicts
- Provider accountability and roles are clear regardless of virtual or bricks and mortar site of care or employment affiliation
- Care protocols and care delivered consistently align with guidelines
- Collaboratively defined clinical care pathways for specific therapeutic areas with partners
- Works with payors to track and report on on-pathway adherence
- Care transitions, including escalations and site of care handoffs, are managed with minimal friction according to proactive workflows
- Ability to collaborate to define and meet quality and accreditation goals
Resources
- Guide to Effective Virtual-First Care (V1C) Transitions (See Necessary Conditions for Clinical and Operational Integration)
- Quickstart Guide to Partnerships between V1C Providers and Accountable Care Organizations (ACOs)
- Guide to Effective Virtual-First Care (V1C) Care Transitions (V1C Patient Co-Management)
Case Studies
- Biofourmis Case Study: Coordinating Virtual Specialty Care for Polychronic Patients
- Byteflies Case Study: Digital Medicine as an Enabler of Effective V1C Care Transitions
- CareHive Case Study: Navigating Patients across the Continuum of Care Transitions
- Heartbeat Health Case Study: V1C Partnering with ACOs for Effective Care Transitions
- Oshi Health Case Study: Achieving Whole-Person Care
- Thirty Madison Case Study: Seamless Downstream Referrals Advance Access to HIV Prevention
- Wellinks Case Study: Integrating High-Value V1C Solutions for Disease Management
Positioned for bi-directional data flow with plan sponsors and health plans:
- Uses Fast Healthcare Interoperability Resources (FHIR) standards for seamless Application Programming Interface (API) integration
- Ability to share data with employee group medical benefit plans and health insurance companies to support activities such as HEDIS or in-network referrals in full compliance with appropriate regulations (e.g., HIPAA)
- Ability to identify and refer patients to other employer-based health programs available to the patient, e.g., Employee Assistance Programs (EAPs)
Resources